Lab 1
Back to Table
of Contents
SHEEP BRAIN DISSECTION: LAB 1
Now we'll begin identifying some prominent features on the surface
of the brain and will also begin to locate and identify cranial nerves I through
VI. Always follow the links to the tables that present
important information about each nerve and its location. Once you
have seen a structure on the monitor, find it on your sheep brain specimen.
Always keep in mind that the practicum will employ actual tissue, so you will
always want to be able to identify important structures on your sheep brain,
not just on the images you see on screen. These images are much larger
than your actual sheep brain, and some images have been altered to insrue that
the structures are clear.
Make a list of important terms and structures to guide your
study. On the practicum, you will be expected to be able to locate, define,
or provide explanatory information about the function of a structure, as appropriate,
for each of the terms that appears in blue in the guide.
The Meninges.
In situ (in place) the living brain and spinal cord are encapsulated
by three membrane sheaths called the meninges.
The outermost membrane is the dura-mater,
tough, fibrous, and translucent. There may be some dura attached to your
specimen, but most of it was likely removed at the time that the brain was extracted
from the skull. As shown in the schematic drawing, the
dura coats the outer surface of the brain.The
middle layer of the meninges is the arachnoid;
it is more delicate than the dura and has a cobweb-like appearance, when the
brain is intact. The  arachnoid
is not visible to you at this time, because the process of preservation produces
shrinkage of the tissue. The subarachnoid space is filled with cerebrospinal
fluid. The innermost meningeal layer, the
pia-mater, is an extremely delicate membrane
that covers the surface of the CNS. It extends into every sulcus and fissure.
In contrast, the dura mater wraps the the surface of the CNS without projecting
into the crevices formed by the mounds of the gyri. Cerebrospinal
fluid (CSF), found in the sub-arachnoid space, that space between
the pia and the arachnoid, is manufactured in specialized tissue called choroid
plexus, which is located at several sites in the CNS, some of which
you will observe later. (N.B. the scale and relationship of the meninges
are distorted in the figure. See your text for a more veridical image.)
arachnoid
is not visible to you at this time, because the process of preservation produces
shrinkage of the tissue. The subarachnoid space is filled with cerebrospinal
fluid. The innermost meningeal layer, the
pia-mater, is an extremely delicate membrane
that covers the surface of the CNS. It extends into every sulcus and fissure.
In contrast, the dura mater wraps the the surface of the CNS without projecting
into the crevices formed by the mounds of the gyri. Cerebrospinal
fluid (CSF), found in the sub-arachnoid space, that space between
the pia and the arachnoid, is manufactured in specialized tissue called choroid
plexus, which is located at several sites in the CNS, some of which
you will observe later. (N.B. the scale and relationship of the meninges
are distorted in the figure. See your text for a more veridical image.)
Functional importance of the
meninges.
CSF and the meninges are designed to protect the brain and spinal
cord from mechanical shock. Without them, or a functionally similar system,
it is conceivable that slight, otherwise insignificant bumps on the head, or
even a mild shaking of the head back and forth, would induce a state of unconsciousness
as the brain was thrust against one side of the skull cavity and then the other.
CSF can be of diagnostic use to neurologists and neurosurgeons. When a
spinal tap is conducted, that is, when CSF is withdrawn from the spinal cord,
several characteristics of the CSF are assayed. Under normal conditions
it should have no color, and it should have no cloudiness or turbidity.
Deviations from these normal conditions are clinically significant (e.g., a
slightly pink and cloudy sample might indicate minute intracerebral hemorraghing).
The meninges, especially the dura mater, greatly impede
visual appreciation of the external features of the brain; so, you must
carefully remove them (but not yet!). The pia mater is very delicate and
adheres to the brain's surface tenaciously; it will take considerable patience
and care to remove it. Wait for instructions from the instructor or lab
assistant on how to remove the dura mater from your specimen, because several
cranial nerves pass through the dura and you want to avoid accidentally removing
them when you remove this protective sheath.
Once you are certain about how to proceed, begin to remove the
dura from the dorsal surface of the brain. The instructor or lab assistant
will help you locate the pituitary gland
on the ventral surface of the brain. It is the prominent and protruding
mass of tissue lying on the ventral midline, just anterior to the brainstem.
It will be necessary to remove the pituitary in order to have an unobstructed
view of some of the features present on the ventral surface of the brain.
It is likely that a variety of tissues will be found proximal to the pituitary.
The tough, transparent material overlaying the pituitary is dura mater, while
the dark brown, porous, and hairlike matter located along the gland's lateral
surfaces is a capillary bed, which is an
appropriate accompaniment considering the operation of the pituitary.
Why do you think a rich capillary bed is located near the pituitary?
Carefully lift the pituitary mass from its caudal end. You will see two
large, flat fiber bundles that are attached to the ventral surface of the brain
and to the dura. These fiber bundles are the oculomotor
nerve, cranial nerve III. Keeping the pituitary mass lifted
away from the ventral surface of the brain, use a pair of scissors to
sever the two branches of the III nerve close to its attachment to the dura,
that is, leave as much of the nerve attached to the brain stem as you are able.
As you lift the pituitary, notice a small, thin tubular structure,
the infundibulum or infundibular stalk,
which joins the pituitary to the base of the brain. It is located
on the midline, anterior to the oculomotor nerves. The stalk will
rupture as you remove the pituitary and will leave a small hole, which represents
the point at which the infundibulum attached the pituitary to the hypothalamus.
Carefully cut any other connective tissue present, lift the pituitary
away, and set it aside. (Do not throw it away; you will be using it in a later
session.) If you perform these actions carefully, you should be able to
preserve many of the cranial nerves that emerge from the ventral surface of
the brain. 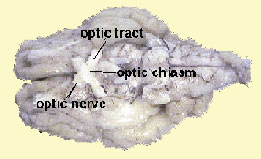
You will also have to remove the dura from the optic
nerve (II) and the optic chiasm.
The optic nerve and the chiasm (which means crossing) can be identified as the
large structures that form an "X" on the ventral surface of the brain.
Proceed cautiously, or you may break off the nerves or damage the chiasm.
Nerves and Features
of the Ventral
Surface of the Brain.
If your dura and pituitary gland have been removed, you
are ready to begin to locate and identify the cranial nerves that remain on
your specimen. One basis for classifying nerves is by location. Spinal
nerves appear entering or exiting the spinal cord and cranial
nerves are found entering or exiting from the brain. A second basis
for classification is by function, that is, whether the nerve is sensory
(afferent) or motor (efferent).
Students often have difficulty remembering whether it is sensory
or motor information that is afferent or efferent and whether it is the dorsal
or ventral root that carries afferent or efferent information. The word,
SAME, and the name, DAVE,
are good mnemonics for keeping this information straight. For example,
the letters of the word SAME can be used to recall that sensory
information is afferent and motor information is efferent. Similarly, the name,
DAVE, can help keep the organization of the spinal roots clear.
|
Sensory
|
|
Dorsal
|
| Afferent |
(information going to the brain) |
Afferent
|
| Motor |
|
Ventral
|
| Efferent |
(information exiting brain and spinal
cord going to muscles and glands) |
Efferent
|
This is a good place to mention the Law
of Roots (also known as the Law of Bell and Magendie). The Law of
Roots states that sensory information enters through the dorsal root of the
cord and motor information exits through the ventral root. There are 31 spinal
nerves and each has a dorsal and a ventral root. Each of the 31 dorsal
roots carry incoming (afferent)
sensory information, while the axons in all 31 ventral
roots carry outgoing(efferent)
motor information to the muscles and glands. The dorsal and ventral roots
join to form mixed spinal nerves that contain
both sensory and motor fibers. Ask the instructor or lab assistant to
show you the model of the human spinal cord, or, better yet, request to see
the preserved human spinal cord tissue to obtain a clear appreciation of this
spinal organization.
Identification of the
Cranial Nerves.
There are 12 pairs of cranial nerves customarily numbered
with the Roman numerals, I to XII. They appear in an approximate rostral
to caudal sequence along the ventral surface of the brain. Refer
to Table
1, for an outline of the functions of all 12 cranial nerves and
some mnemonics to help you remember their names and numbers. You will
find this Table useful in your studying. On the practicum, you will be
expected to be able to indicate whether a given nerve is sensory, motor, or
both. In addition, you must know what functions each of the 12 nerves
serve. You will have to identify, by location, only cranial nerves I through
VI.
On the ventral aspect of your specimen, at the very anterior
limit, locate the two pad-like flaps of tissue that are the olfactory
bulbs, the second-order neurons of cranial nerve I.
 Caudal
to the olfactory bulbs, along the midline, note the "X" formed by two fairly
substantial fiber groups. The fibers anterior to the intersection of the
"X," are optic
nerve fibers. The intersection of the 'X,' is the optic
chiasm, while fibers caudal to the optic chiasm
are optic tract
fibers. Follow the links for information about the optic chiasm and the optic
nerve.
Caudal
to the olfactory bulbs, along the midline, note the "X" formed by two fairly
substantial fiber groups. The fibers anterior to the intersection of the
"X," are optic
nerve fibers. The intersection of the 'X,' is the optic
chiasm, while fibers caudal to the optic chiasm
are optic tract
fibers. Follow the links for information about the optic chiasm and the optic
nerve.
Take time now to
consider the facts about the optic chiasm that were presented in the table.
Do you understand
where the optic fibers originate
how some fibers crossover as they begin their journey to occipital (visual)
cortex?
Stop, now, and draw
a figure in the margin of your dissection guide that demonstrates how these fibers
project to occipital cortex.
Do not proceed unless you know :
the difference between the optic
nerve and optic tract
whether the optic nerve or optic tract contains ipsilateral,
or contralateral fibers, or both).
Just caudal to the optic tracts
are two very large bundles of fibers running parallel to the lateral surfaces
of the brain. These large fiber bundles are called the cerebral
peduncles. The cerebral peduncles are large bundles of axons
coming from cell bodies located in motor cortex. These cell bodies are called
pyramidal cells. As the pyramidal
cell axons leave motor cortex, they are arranged in a large crescent-shaped
structure called the internal capsule. As
the axons make their descent to their final destination, the spinal cord, they
merge into the two, tight bundles of fibers seen on the ventral surface of the
brain, where they are called the cerebral peduncles. The axons continue
to course downward and disappear beneath the pons. The fiber bundle reappears
as striations on the external surface of the medulla, where they are called
the pyramidal tract. Once these fibers reach the spinal cord, they are called
the cortico-spinal tract. (Remember the
rule regarding the naming of nerves and tracts? The first part of the name indicates
where the fibers begin (or are coming from) and the second half of the name
specifies the destination.) The axons in this long pathway from motor cortex
to internal capsule, internal capsule to cerebral peduncles, cerebral peduncles
to pyramidal tract and spinal cord comprise one of the major motor pathways
in the CNS. This motor system, called the pyramidal
motor system, is largely responsible for intentional movement. Christopher
Reeves, the actor who suffered a severe spinal cord injury, is paralyzed, because
the axons in his cortico-spinal tract were severed in his accident. As a result,
the signals from his motor cortex to his spinal cord have been disrupted; his
pyramidal motor system axons no longer communicate with the muscles of his body
to produce movement.
There are two other important components that are involved
in the production of the many complex movements we can exhibit: the extra-pyramidal
system and the cerebellum. We'll learn more about the contributions of
these two aspects of our motor systems later.
On the surface of each peduncle, you should find cranial nerve
III, the oculomotor
nerve, which supplies four eye muscles.
Two 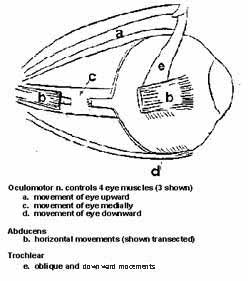 muscles are marked
by the letters: a and d. As you can surmise, these muscles move the eye
up (elevation) and down (depression). A third muscle, marked 'c' in the
figure, is attached to the medial surface of the eyeball and rotates the eye
inward toward the nose (adduction). You activate this muscle when you
cross your eyes. The fourth muscle supplied by the oculomotor nerve moves the
eye upward and outward toward the temple (extorsion). This fourth muscle
is not shown.
muscles are marked
by the letters: a and d. As you can surmise, these muscles move the eye
up (elevation) and down (depression). A third muscle, marked 'c' in the
figure, is attached to the medial surface of the eyeball and rotates the eye
inward toward the nose (adduction). You activate this muscle when you
cross your eyes. The fourth muscle supplied by the oculomotor nerve moves the
eye upward and outward toward the temple (extorsion). This fourth muscle
is not shown.
Looking postero-laterally, between the
cerebral hemispheres and the cerebellum, find a very thin, thread-like nerve,
the trochlear
nerve, cranial nerve IV.
It exits the dorsal surface of the brainstem, but courses immediately ventralward;
it is often hidden by the bulk of the the trigeminal nerve, cranial nerve V.
The muscle marked 'e' in the figure is supplied by the trochlear nerve
which moves your eye down and in toward the nose (intorsion).
At the anterior limit of the medulla (that section
of the brain located caudal to the pons and anterior to the spinal cord)
you will find several cranial nerve processes aligned in
a near transverse manner. The most medial of these is cranial
nerve VI, the abducens,
which serves the external rectus muscle of the eye that allows you to move
your eyes outward toward the temple (abduction). The external rectus of
the eye is marked by the letter 'b' in the Figure. Note that the nerve has
been cut in the figure to reveal the muscle marked 'c'.
Now locate cranial
nerve V, the trigeminal;
it will be seen as a relatively thick fiber bundle near the lateral-most
junction of the pons and medulla.
It may be that the trigeminal nerve has been torn away from your specimen; if
this is so, locate it using this ventral
view of the brain.
Cranial nerves VII through XII were quite likely
stripped from your sheep brain. Therefore, you will not be responsible for
locating these nerves during the practicum, but you will need to know whether
these nerves are sensory or motor, or mixed, and what functions they subserve.
See Table 1 for the name,
number, and function of all the cranial nerves including nerves VII to XII.
This
completes Lab 1 of the dissection
Here are some hints to aid you in studying for the
practicum:
- Make a list
of all the terms and structures that appear in blue in the text. Make certain
that you can define, identify, or locate each structure as applicable.
- Index cards
can be useful. On one side of the card write the
name of a term or structure. On the opposite side of the card record
relevant information. For example, for the cerebral peduncles you would
have the name of the term on one side, on the other you might record:
large fiber bundle running parellel to the lateral surfaces of the brain.
Contain axons from cells in motor cortex sending information to spinal cord.
Cranial nerve III exits from its surface. You can use these cards to
guide your study. On some occasions, look at the name of the structure,
test whether you can locate the structure on the your sheep brain. Can
you provide relevant information about this structure? The next time
you study look at the descriptive information on one side of the card, can
you name the structure from its description? Can you locate it?
- Identify
all the structures located on the ventral surface of
your sheep brain; now identify the structures on the specimen without
using any images in the dissection as an aid.
- Use Table 1
to help you learn the function of each of the cranial nerves.
- Quiz one
another. Pay particular attention to items that are not obvious or readily
understood.
- Take the Practice
test.
- Refer to a text book
in Biological Psychology or Behavioral Neuroscience for further clarification,
if necessary. Make note of areas of confusion that arise during your
study periods. Consult with the instructor or the lab assistants to
resolve those areas of difficulty as soon as possible.
Back to
Table of Contents
 arachnoid
is not visible to you at this time, because the process of preservation produces
shrinkage of the tissue. The subarachnoid space is filled with cerebrospinal
fluid. The innermost meningeal layer, the
pia-mater, is an extremely delicate membrane
that covers the surface of the CNS. It extends into every sulcus and fissure.
In contrast, the dura mater wraps the the surface of the CNS without projecting
into the crevices formed by the mounds of the gyri. Cerebrospinal
fluid (CSF), found in the sub-arachnoid space, that space between
the pia and the arachnoid, is manufactured in specialized tissue called choroid
plexus, which is located at several sites in the CNS, some of which
you will observe later. (N.B. the scale and relationship of the meninges
are distorted in the figure. See your text for a more veridical image.)
arachnoid
is not visible to you at this time, because the process of preservation produces
shrinkage of the tissue. The subarachnoid space is filled with cerebrospinal
fluid. The innermost meningeal layer, the
pia-mater, is an extremely delicate membrane
that covers the surface of the CNS. It extends into every sulcus and fissure.
In contrast, the dura mater wraps the the surface of the CNS without projecting
into the crevices formed by the mounds of the gyri. Cerebrospinal
fluid (CSF), found in the sub-arachnoid space, that space between
the pia and the arachnoid, is manufactured in specialized tissue called choroid
plexus, which is located at several sites in the CNS, some of which
you will observe later. (N.B. the scale and relationship of the meninges
are distorted in the figure. See your text for a more veridical image.)
 Caudal
to the olfactory bulbs, along the midline, note the "X" formed by two fairly
substantial fiber groups. The fibers anterior to the intersection of the
"X," are
Caudal
to the olfactory bulbs, along the midline, note the "X" formed by two fairly
substantial fiber groups. The fibers anterior to the intersection of the
"X," are 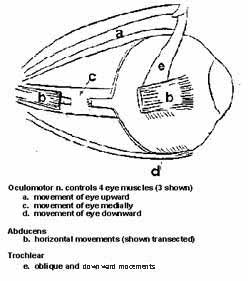 muscles are marked
by the letters: a and d. As you can surmise, these muscles move the eye
up (elevation) and down (depression). A third muscle, marked 'c' in the
figure, is attached to the medial surface of the eyeball and rotates the eye
inward toward the nose (adduction). You activate this muscle when you
cross your eyes. The fourth muscle supplied by the oculomotor nerve moves the
eye upward and outward toward the temple (extorsion). This fourth muscle
is not shown.
muscles are marked
by the letters: a and d. As you can surmise, these muscles move the eye
up (elevation) and down (depression). A third muscle, marked 'c' in the
figure, is attached to the medial surface of the eyeball and rotates the eye
inward toward the nose (adduction). You activate this muscle when you
cross your eyes. The fourth muscle supplied by the oculomotor nerve moves the
eye upward and outward toward the temple (extorsion). This fourth muscle
is not shown.